Understanding the Role of Botox for Jaw Clenching: A Comprehensive Guide


Bruxism, or jaw clenching, is a frequent ailment that causes teeth to grind or clench during sleep.
Jaw clenching, medically known as bruxism, is a common condition characterized by involuntary grinding or clenching of the teeth, often occurring during sleep. While the exact causes of bruxism vary, factors such as stress, anxiety, misaligned teeth, and certain medications can contribute to its onset. Chronic jaw clenching not only leads to dental issues but also contributes to headaches, jaw pain, and temporomandibular joint (TMJ) disorders. Fortunately, Botox, commonly associated with cosmetic enhancements, has emerged as an effective therapeutic option for managing jaw clenching. In this comprehensive guide, we’ll delve into the mechanisms of bruxism, explore the benefits of Botox for jaw clenching, and discuss its application as a therapeutic intervention.
Understanding Jaw Clenching (Bruxism)
Bruxism encompasses the involuntary grinding, gnashing, or clenching of teeth, often occurring during sleep. While occasional tooth grinding may not pose significant concerns, chronic bruxism can lead to a host of dental, muscular, and psychological issues. Common symptoms of bruxism include tooth wear, jaw pain, headaches, and TMJ disorders. The etiology of bruxism is multifactorial, involving a combination of psychological, physiological, and anatomical factors. Stress, anxiety, malocclusion, and sleep disorders are among the contributing factors implicated in bruxism development.
The Role of Botox in Managing Jaw Clenching
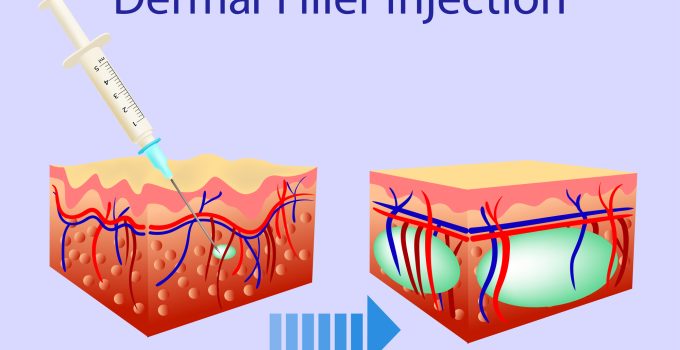
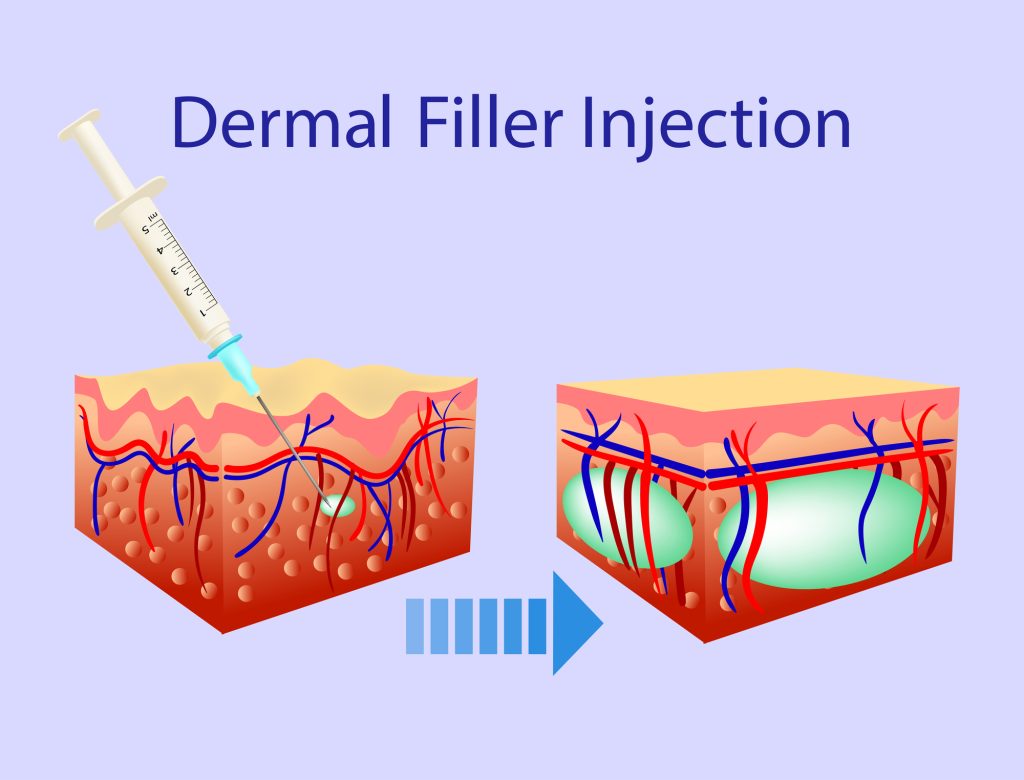
Botox, derived from the botulinum toxin, is widely recognized for its muscle-relaxing properties and is primarily used in cosmetic treatments to reduce wrinkles and fine lines. However, Botox’s therapeutic applications extend beyond aesthetics, encompassing various medical conditions, including bruxism. By inhibiting the release of acetylcholine, a neurotransmitter responsible for muscle contractions, Botox effectively relaxes the muscles involved in jaw clenching, thereby alleviating associated symptoms and complications.
Benefits of Botox for Jaw Clenching
- Muscle Relaxation: Botox injections target the masseter and temporalis muscles, the primary muscles involved in jaw clenching. Botox helps mitigate the intensity and frequency of clenching episodes by inducing muscle relaxation and reducing associated muscle tension and discomfort.
- Pain Relief: Chronic jaw clenching often leads to jaw pain, headaches, and TMJ disorders. Botox injections offer significant pain relief by attenuating muscle hyperactivity and alleviating tension-related symptoms, thereby enhancing overall comfort and well-being.
- Prevention of Dental Damage: Bruxism can result in tooth wear, fractures, and enamel erosion, necessitating extensive dental interventions. Botox therapy helps prevent dental damage by reducing the force exerted during clenching episodes, preserving tooth structure, and minimizing the need for invasive dental procedures.
- Improved Sleep Quality: Bruxism frequently occurs during sleep, disrupting sleep patterns and contributing to daytime fatigue. By reducing the severity of nocturnal clenching, Botox promotes better sleep quality, enabling individuals to experience restful and rejuvenating sleep without the interruptions caused by bruxism-related symptoms.
- Enhanced Quality of Life: The debilitating effects of bruxism extend beyond physical discomfort, impacting emotional well-being and quality of life. Botox therapy offers a holistic approach to bruxism management, addressing both the physical and psychological aspects of the condition and empowering individuals to enjoy a higher quality of life.
The Botox Procedure for Jaw Clenching
A skilled healthcare professional must follow a meticulous process when administering Botox injections for jaw clenching. During the procedure, the provider identifies the target muscles responsible for jaw clenching and administers precise injections into the masseter and temporalis muscles. The dosage and injection sites are customized based on the individual’s unique anatomy and treatment goals. Following the procedure, patients may experience mild discomfort and temporary swelling at the injection sites, which typically resolves within a few days.
Post-Treatment Care and Follow-Up
After receiving Botox injections for jaw clenching, patients are advised to adhere to post-treatment care guidelines to optimize treatment outcomes and minimize potential complications. This may include avoiding strenuous physical activities, refraining from excessive jaw movements, and applying ice packs to reduce swelling. Additionally, patients are encouraged to attend follow-up appointments to assess treatment efficacy, address any concerns, and determine the need for additional injections based on individual response and symptom severity.
Conclusion
Botox therapy offers a safe, effective, and minimally invasive approach to managing jaw clenching, relieving associated symptoms, and improving overall quality of life. Botox helps alleviate jaw pain, headaches, and dental complications by targeting the underlying muscle hyperactivity responsible for bruxism, enabling individuals to experience enhanced comfort and well-being. If you’re struggling with the debilitating effects of jaw clenching, consider consulting with a qualified healthcare professional to explore the potential benefits of Botox therapy and embark on the journey towards a healthier, more comfortable smile.