Recently, injectable neurotoxin therapies, usually associated with cosmetic procedures, have shown potential for migraine relief.
Migraines are not just headaches; they are debilitating neurological conditions that can significantly impair one’s quality of life. For those who suffer from chronic migraines, the quest for relief often leads to a multitude of treatments, ranging from medications to lifestyle changes. However, for some, traditional methods may fall short of providing adequate relief. In recent years, injectable neurotoxin treatments, commonly associated with cosmetic procedures, have emerged as a promising option for managing chronic migraines. This article delves into the efficacy, mechanism of action, qualification criteria, side effects, insurance coverage, and overall impact of injectable neurotoxin treatments, such as Botox®, in alleviating the burden of chronic migraines.
Understanding Injectable Neurotoxin Treatments for Migraines
When discussing injectable neurotoxin treatments like Botox® for migraines, it’s crucial to dispel the notion that these injections are solely for cosmetic purposes. While Botox® is renowned for its use in minimizing facial wrinkles, it has also gained FDA approval for the treatment of chronic migraines. Unlike medications that are taken during a migraine attack, injectable neurotoxins work as a preventive measure, aiming to reduce the frequency and severity of migraines.
Mechanism of Action
The mechanism by which injectable neurotoxins alleviate migraines lies in their ability to modulate pain signaling pathways. Research suggests that these neurotoxins inhibit the release of neurotransmitters involved in pain transmission and alter the communication between the brain and nerves responsible for migraine generation. Specifically, Botox® injections target peripheral nerves in areas such as the head, neck, and shoulders, where migraine signals originate. By interfering with the transmission of pain signals, Botox® helps reduce the frequency and intensity of migraine attacks.
Treatment Protocol
The treatment protocol for injectable neurotoxin therapy typically involves a series of injections administered every 12 weeks. Each session consists of 31 injections, with five units of Botox® injected into specific sites associated with migraine pathology. While the procedure itself may cause minimal discomfort, lasting only about 20 minutes, the benefits may not be immediately apparent and may require several treatment cycles to manifest fully.
Qualification Criteria
Not every migraine sufferer is a candidate for injectable neurotoxin treatments. Qualification for these therapies is determined based on several factors, including the frequency, severity, and duration of migraines, as well as the individual’s response to previous treatment modalities. It is essential for individuals considering neurotoxin injections to consult with their healthcare provider, who may refer them to a headache specialist or neurologist for a comprehensive evaluation.
Side Effects
Like any medical intervention, injectable neurotoxin treatments carry potential side effects. These can range from temporary pain and swelling at the injection site to more serious complications, such as neck pain and changes in facial symmetry. Additionally, there is a risk of rare but severe adverse reactions, including difficulty breathing, swallowing, or speaking. Patients should discuss these risks thoroughly with their healthcare provider before undergoing treatment.
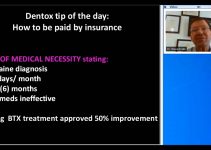
Insurance Coverage
One common concern for individuals considering injectable neurotoxin therapy is whether it will be covered by insurance. Fortunately, since these treatments are FDA-approved for chronic migraines, most insurance plans provide coverage. However, specific criteria may need to be met, and navigating the approval process may require assistance from healthcare providers.
Improving Quality of Life
For many chronic migraine sufferers, injectable neurotoxin treatments offer a ray of hope amidst the darkness of debilitating pain. By reducing the frequency and severity of migraines, these therapies can significantly improve one’s quality of life. Reports from patients who have undergone Botox® injections for migraines often highlight a decrease in migraine frequency between sessions and an overall improvement in their ability to function and engage in daily activities.
Conclusion
Chronic migraines pose a significant burden on individuals, affecting every aspect of their lives. While traditional treatment modalities may provide relief for some, others continue to search for more effective solutions. Injectable neurotoxin treatments like Botox® offer a novel approach to migraine management, targeting the underlying mechanisms of migraine pathology. While not suitable for everyone, these treatments have demonstrated efficacy in reducing migraine frequency and improving the quality of life for many sufferers. By consulting with healthcare providers and exploring available options, chronic migraine sufferers can take proactive steps towards reclaiming control over their lives and finding relief from the relentless grip of migraines.