Exploring the Potential of Botox for Arthritis Pain Relief

Botox relieves arthritis pain by targeting and relaxing joint-pain-causing muscles.
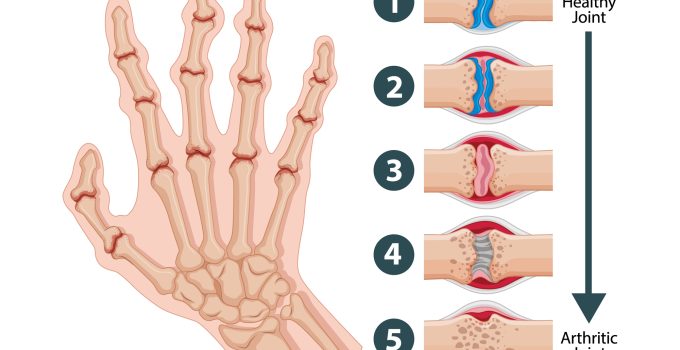
Botox, primarily known for its cosmetic applications in reducing wrinkles and fine lines, is increasingly being investigated for its therapeutic potential in addressing various medical conditions. Among these is arthritis, a chronic condition characterized by joint inflammation and pain. While traditionally associated with cosmetic enhancements, Botox’s ability to relax muscles has sparked interest in its potential to alleviate arthritis pain and improve mobility. This article will delve into the emerging research on Botox for arthritis pain relief, its mechanisms of action, potential benefits, and considerations for those considering this treatment option.
Understanding Botox for Arthritis Pain Relief
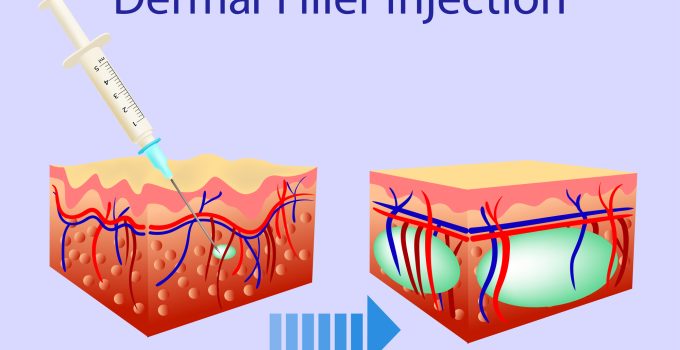
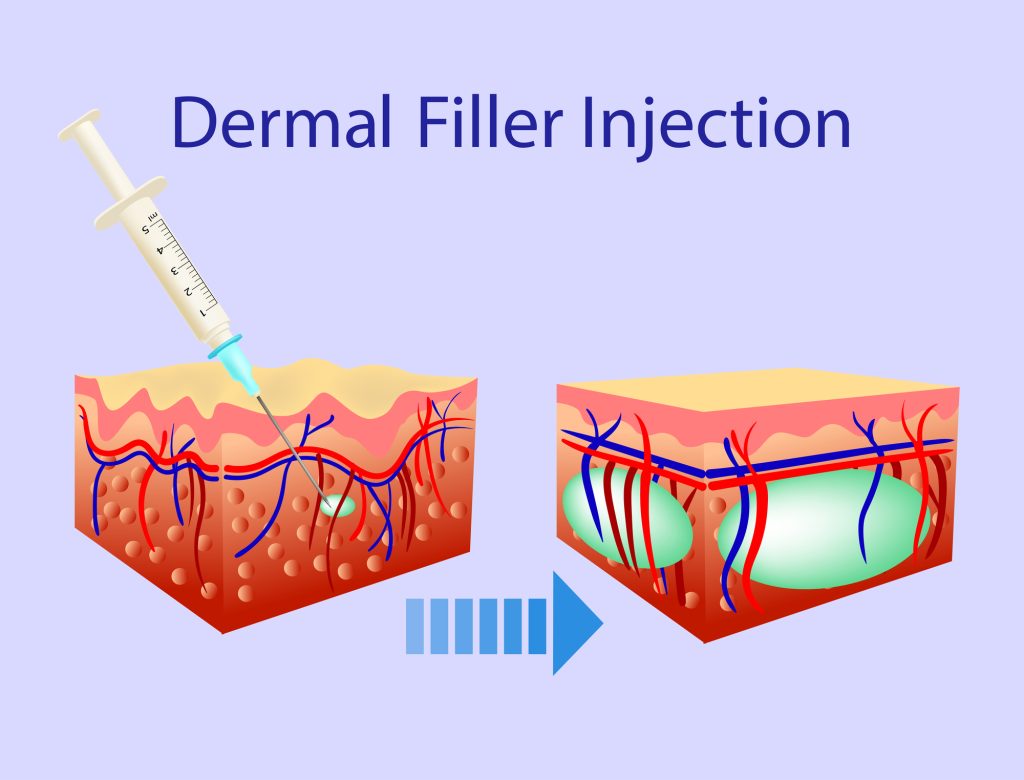
The bacterium Clostridium botulinum produces botox, also known as botulinum toxin type A, which is a neurotoxin. When injected into muscles, it temporarily blocks nerve signals that control muscle contractions, leading to muscle relaxation. While its cosmetic applications are well-established, Botox’s therapeutic uses have expanded over the years, including treatment for migraines, muscle spasms, and overactive bladder.
The concept of using Botox for arthritis pain relief revolves around its ability to target and relax specific muscles that contribute to joint discomfort. By reducing muscle tension and spasms, Botox may alleviate pain associated with arthritis and improve joint mobility. While the treatment is not a permanent solution, with effects typically lasting for several months, even temporary relief can significantly enhance the quality of life for arthritis sufferers.
Can Botox injections relieve arthritis pain?
Preliminary studies and anecdotal evidence suggest that Botox injections may offer relief from arthritis pain for some individuals. Patients have reported improvements lasting up to four months following treatment. While this duration is not permanent, it represents a significant improvement for individuals who endure daily arthritis symptoms.
It’s important to note that Botox’s effectiveness in relieving arthritis pain is still being investigated through ongoing research. While promising, further studies are needed to understand the optimal dosages, injection sites, and patient selection criteria for maximizing therapeutic outcomes. Additionally, individual responses to Botox treatment may vary, highlighting the importance of personalized care and evaluation by qualified medical professionals.
Exploring Botox’s Versatility in Medical Treatment
Beyond its well-known cosmetic applications, Botox has garnered FDA approval for treating various medical conditions, reflecting its versatility and therapeutic potential. In addition to arthritis pain relief, Botox has demonstrated efficacy in managing migraines, muscle spasms, and urinary incontinence, among other conditions.
This expanding repertoire of medical uses underscores Botox’s multifaceted nature and the ongoing exploration of its therapeutic benefits. As researchers delve deeper into Botox’s mechanisms of action and its effects on different physiological processes, new avenues for medical intervention continue to emerge.
Considerations for Botox Treatment
While Botox holds promise as a potential treatment for arthritis pain, several considerations should be considered before undergoing this procedure. First and foremost, only qualified healthcare professionals like doctors, nurses, or dermatologists should administer Botox injections. Seeking treatment from reputable medical providers ensures safety and optimal treatment outcomes.
Additionally, individuals considering Botox for arthritis pain relief should discuss their medical history and treatment goals with a healthcare provider. Not everyone may be suitable for this treatment, and alternative therapeutic options should be explored based on individual needs and preferences.
Additionally, it’s crucial to have reasonable expectations for the duration and degree of pain relief that Botox injections will provide. While some patients may experience significant improvements, others may find more modest benefits or require additional interventions to manage their arthritis symptoms effectively.
Future Directions and Conclusion
As research into Botox’s potential for arthritis pain relief continues to evolve, it promises to offer a non-invasive and temporary solution for alleviating joint discomfort and improving mobility in arthritis patients. While further studies are needed to validate its efficacy and refine treatment protocols, the growing body of evidence suggests that Botox may emerge as a valuable adjunctive therapy for managing arthritis symptoms.
In conclusion, exploring Botox’s therapeutic applications beyond cosmetic enhancements represents a fascinating medical research and innovation area. While arthritis pain relief is still in the early stages of investigation, the promising results observed thus far offer hope for a breakthrough in arthritis management. With continued research and clinical advancements, Botox may soon become a valuable tool in the comprehensive treatment approach for arthritis and other chronic pain conditions.